Invest in the solution
6.1 The nursing workforce: a good investment
‘Over the past three decades nursing has been seen as a cost as opposed to an investment in healthcare, with health employment viewed as ‘consumption’ ~ High-Level Commission on Health Employment and Economic Growth, 2016
NZNO and nursing in general have advocated strongly that investment in nursing is an investment in health and in the economy. NZNO works to raise awareness of the substantial and cost effective contribution of nursing to improving health outcomes for New Zealanders.
Research confirms the importance of investment in nursing for quality, safe and accessible healthcare. Investment in more staff, better skill mix, education and competencies have been associated with overall cost savings, better patient outcomes, reduced mortality levels and greater patient satisfaction.
It is crucial the Government recognises that expenditure on health is an investment and not an economic drain.
Healthy populations create economic growth, yet in too many parts of the world health spending is being cut and there is under investment in health services.
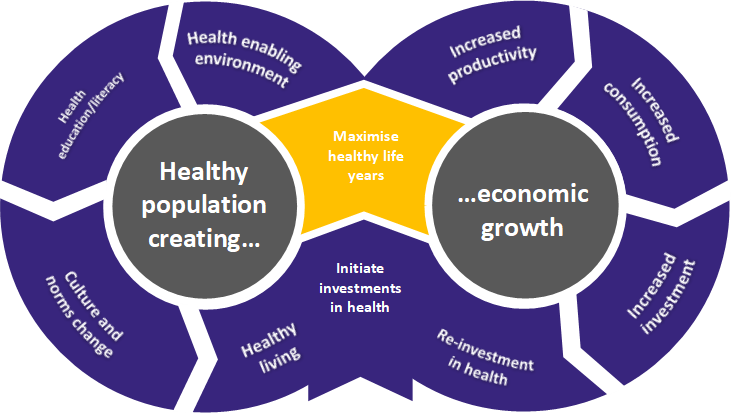
Source: International Council of Nurses, 2017
Nurses have a crucial role in providing quality, accessible healthcare, and nursing has a responsibility to ensure Aotearoa New Zealand secures the potential clinical, social and economic benefits of the profession.
Strategic actions
NZNO will
- Invest in research that directly identifies the impact of nursing. Current evidence in this area needs to be more robust
- Collaborate with the global Nursing Now campaign
- Support continued research to demonstrate care effective and cost- effective services across the health continuum. It will do this through the NZNO policy and research team, scholarship funds and publishing research
- Role model and support nursing leadership to demonstrate and promote the value and cost effectiveness of nursing, including planning and policy development
- Engage a health economist (as required) to facilitate the articulation of nursing as a care-effective and cost-effective workforce for Aotearoa New Zealand
- Work with the Productivity Commission to identify case studies of value in nursing.
6.2 Transforming the nursing workforce
Nursing is the largest regulated health workforce in Aotearoa New Zealand, representing over 50 per cent of the regulated workforce population. Nurses also supervise the largest unregulated health workforce (health care assistants, caregivers and support workers).
Future nursing services must focus on the social determinants of health, health promotion, disease prevention, primary health care and services that are people centred and community based. These services must be in areas of high needs and underserved populations.
Nursing has the capacity, the skills (and potential for upskilling), and the adaptability to support the increasing number of people with health, social and psychological concerns, who are unable to access services due to cost, accessibility, literacy or lack of culturally appropriate services.
Nursing can be an effective health safety net for people who are not accessing GP services. Failure to invest in this safety net will be a wasted opportunity and create greater health inequities and be more expensive in the longer term.
The demographics of nurses are well known and are not changing in a positive or timely way:
- Age of nurses: 43 per cent of nurses are over the age of 50(including nursing faculty
- Men in nursing: Eight per cent of nurses are men (minimal movement over time)
- Māori in nursing: Seven per cent of the total nursing workforce is Māori compared to 15 per cent of the New Zealand population
- Internationally Qualified nurses: 27 per cent of the Aotearoa New Zealand nursing workforce are internationally qualified nurses – higher than any other OECD country.
The headline concerns for the nursing workforce in Aotearoa New Zealand:
- The lack of investment and resources to create a coherent national nursing workforce strategic plan that is current, cogent, and has a timeline for implementation is reprehensible
- The absence of a Māori nursing strategic plan and the resources to support and implement it is equally lamentable
- Less than 100 per cent employment for graduate nurses and not all graduate nurses have access to a nurse -entry-to-practice programme (or equivalent)
- Māori and Pacific nurses are under-represented for the populations they serve
- 50 per cent of the nursing workforce will have retired by 2035
- A dependence on internationally qualified nurses
- Persistent and serious underfunding for postgraduate nursing education.
6.3 National nursing workforce strategy – Health Workforce New Zealand
Health Workforce New Zealand (HWNZ) was established as a MoH business unit in 2009. Despite making a significant contribution to HWNZ through initiatives such as the Nursing Workforce Advisory Group and having a nurse as chairperson, results and outcomes for nursing have been few. Achievement of priority objectives for nursing needs to be accelerated and made visible through HWNZ.
The National Nursing Organisation’s 2014 nursing workforce report to HWNZ outlined nursing workforce strengths and challenges, and laid the foundation for a future-oriented, “fit-for-purpose” nursing workforce. Progress against this report has been limited.
Significant gains have been made in advanced practice enabling nurses to work to the top of their scope. Registered nurse prescribing and the increasing cohort of nurse practitioners is encouraging. These developments must be fast tracked to reach a critical mass as soon as possible. Changes to the model of care need to occur simultaneously so disparities in health can be addressed.
Strategic actions
NZNO will:
- Advocate strongly for the development and implementation of a national nursing workforce strategy and, investment in a Māori nursing workforce strategy
- Advocate strongly for the appropriate resourcing of these workforce strategies, so it can be completed within an accelerated timeframe.
Nursing workforce data and information
Accurate, timely and relevant nursing workforce data should be available from a single, accountable source. This has been challenging to achieve and needs to be resolved urgently by HWNZ to underpin further planning.
Strategic actions
NZNO will:
- Advocate strongly with relevant agencies for dedicated resources for the collection, processing, and protection of nursing workforce data via a timely, relevant and functional system methodology.
6.4 Entering the nursing profession
Aotearoa New Zealand requires a nursing workforce. more representative of the population it serves. All health professions are competing for their future workforces and nursing needs to be seen as a very attractive career option.
The image of nursing is often not contemporary or accurate. The nursing profession must be able to articulate the unique role and practice of nurses.
“The lack of accurate public information about nurses and their work allows insidious stereotypes to persist” ~ Buresh and Gordon, 2013.
There is no single agency responsible for this work, and promotion of nursing as a desired career is often variable, ad hoc and under-invested.
Strategic actions
NZNO (including the National Student Unit and Te Runanga Tauira) in partnership with Nurse Educators in the Tertiary Sector and other relevant parties will:
- Raise awareness in secondary schools and improve uptake in science subjects required/desirable for health careers
- Promote relevant and accurate resources for career guidance counsellors (often teachers whose knowledge base and resources vary and may be outdated)
- Engage with Careers New Zealand and tertiary providers to develop and distribute: a) career guidance resources that target mature students, b) career guidance resources oriented to Māori and Pacific peoples
- Publicise Māori nursing role models.
6.5 Internationally qualified nurses
Aotearoa New Zealand has an over-reliance on short-term, high-turnover immigration to fill nursing skills shortages. This is accompanied by under-employment of new graduates and a lack of investment in nursing career pathways. NZNO believes in sound ethical planning for a sustainable workforce.
Strategic actions
NZNO will continue to advocate for:
- Long-term workforce planning to avoid volatile swings in labour demand and supply, and to meet projected skill shortages
- Development of a stable, self-sustainable workforce consistent with ICN policy, including supported strategies for nurse retention and internationally qualified nurse (IQN) retention, and will work with employers to support IQNs starting work Aotearoa New Zealand.
6.6 Graduate nurses
NZNO has a longstanding policy that every RN or EN should be able to get work and have access to a specifically prepared graduate programme. Nurses have invested heavily in terms of time and money to gain a degree and register as a nurse but face variable job prospects on registration.
The situation for nursing graduates contrasts starkly with medical graduates who are guaranteed a place in a first-year postgraduate programme. Results from Advanced Choice of Employment (ACE) intakes from 2014 to 2017 show that 60 to 70 per cent of new graduates are gaining employment in a NETP or nurse-entry-to-specialist-practice (NESP) programme, leaving approximately 400 new graduates in the ‘talent pool’ each year. This indicates very little progress in NZNO's aspiration for 100 per cent of new graduates to be employed in a NETP or NESP programme.
A note of caution needs to be expressed about the actual percentage of successful applicants; while some are employed in NETP or NESP via an electronic match, some are employed from the ‘talent pool’ and may or may not be on a NETP or NESP programme.
The success rate for Māori new graduates is similar to that of the overall pool. The Pacific graduate success rate is slightly lower.
Significant fluctuations in the number of placements available and the numbers placed also suggests further work is required to increase the number of NETP placements in primary care. Given the focus on health service integration and delivering care closer to home, this requires attention.
Current actions
- NZNO has called for 100 per cent employment of all graduate nurses in a fully funded NETP or NESP programme and will continue to advocate for a “grow our own” policy for graduate recruitment.
Strategic actions
NZNO will:
- Advocate for graduate nurse employment and NETP/NESP places to be recorded as part of a director of nursing dashboard
- Advocate for an improved data repository on graduate nurse employment, particularly those graduates who are unsuccessful in gaining a funded NETP or NESP place
- Advocate for all graduate nurses, ENs and midwives to have funded access to a NETP or NESP programme. ENs do not currently have access to the equivalent support into practice programme).
6.7 Professional nursing development - postgraduate funding
Postgraduate education funding for nursing has been inequitable since its inception. HWNZ has had responsibility for distributing postgraduate education funding for registered health professionals since 2009.
The table below indicates medical hegemony is alive and well in Aotearoa New Zealand.
| Allocation of postgraduate funds to doctors and nurses |
| |
Medical professionals |
Nursing professionals |
| Number |
15,366 |
50,356 |
| Funding |
$107 million |
$14 million |
| Funding per person |
$6,963 |
$278 |
| Funding change 2017 |
5% increase |
No increase |
Adapted from: Kai Tiaki. Vol. 2. March 2017. NZNO.
Postgraduate nursing applications far exceed available funding. It is critical the underlying causes of any under spend in nursing postgraduate funding are identified and remedied, whether these stem from the funding structure, application process, timing limitations or other barriers.
The broad vision for HWNZ postgraduate nursing education is: Working in partnership with key stakeholders to deliver a transparent and consistent model of funding for postgraduate nursing training that will enable nurses to improve health outcomes and disparities of New Zealanders.
HWNZ reviewed the current model of funding distribution for postgraduate education in 2017. The question of how the total fund is increased and the proportion of funding increase for nursing is unstated. It is imperative nursing is involved in strategic decision-making and every stage of implementation for any new funding approach, to ensure historical funding inequities are not continued in a new funding model. HWNZ’s vision will not be fulfilled unless this is achieved in a timely manner.
Strategic actions
NZNO will:
- Ensure the review of the funding allocation model is open, transparent and has input from nursing to correct the current inequities
- Advocate for more postgraduate funding, proportionate to nursing numbers
- Actively monitor outcomes of contestable funding streams for postgraduate studies.
6.8 Māori nursing workforce
An aspirational Māori workforce goal with no further commitment, funding, or implementation strategy is unacceptable. Of equal concern, are the ongoing pay inequities for Māori nurses working within the Māori provider organisations. Pay equity and action towards a cogent realistic Māori nursing workforce strategy MUST be the highest priority to progress Māori nursing.
Nurses working for Māori providers are paid up to 25 per cent less than their counterparts in DHBs; yet it is DHBs who fund the Māori providers. This situation, although complex, could be remedied by different contractual arrangements, if there was the political will to do so.
The intention and timeliness of funding agencies to remedy this situation will be the litmus test of how committed Aotearoa New Zealand is to really addressing the health needs of Māori.
Māori health disparities will continue until there is a critical mass of Māori nurses employed by Māori and iwi providers, who are paid equitably and well supported professionally. The cost of inaction is unacceptable.
Nurses employed by Māori and iwi providers work well when they:
- Have pay parity with colleagues working in DHBs
- Have access to cultural supervision and paid professional supervision
- Are in a supportive managerial structure and environment in which nursing practice is encouraged and valued
- Work with an appropriate balance between RNs and kaiawhina workforce
- Have access to Māori nursing role models, mentoring and coaching
- Have a career development pathway
- Work with intermediate and distal outcomes, across health and social sectors
- Established positive networks with health and social sector agencies
- Have access to funding for postgraduate education and the on-the-job practice requirements of their role
- Are encouraged and supported to learn and speak te reo
- Work within a Māori practice framework, eg the Meihana model
- Are able to practise relevant cultural healing modalities.
Strategic actions
NZNO will:
- Lead multi-agency initiatives to increase the Māori nursing workforce to at least 15 per cent of the total nursing workforce - reflecting the Māori population in Aotearoa New Zealand. This will be achieved by 2030. A dedicated Māori nursing strategy needs to be developed by HWNZ to support the achievement of this goal.
6.9 Pacific workforce
New Zealand’s Pacific population is growing about three times faster than other groups in Aotearoa New Zealand. The Pacific population is very dynamic in Aotearoa New Zealand, and the cultural world views, beliefs and values are diverse and evolving.
As per Aotearoa New Zealand’s Pacific population in general, the Pacific nursing workforce has a significantly younger age profile than the overall nursing workforce. This provides a positive counterbalance to the ageing profile of the Aotearoa New Zealand nursing workforce.
Nearly half of Pacific nurses identify with more than one ethnic group. It is therefore important to acknowledge that “one size” does not fit all, that the Pacific nursing workforce reflects the ethnicities of Pacific people in Aotearoa New Zealand, and the changing nature of what it means to be from the Pacific in Aotearoa New Zealand. A culturally competent workforce that can transcend age and generational issues is also vitally important.
The Pacific population is youthful, culturally and ethnically diverse, and highly urbanised. There is significant work to be done to encourage entry to the nursing profession for Pacific people, to ensure growth and sustainability across the health sector.
NZNO supports the recommendations in the Pacific Health Workforce Service Forecast: Report to Health Workforce New Zealand and the Ministry of Health and agrees with the forecast and planning initiatives, especially in relation to existing and future Pacific nurses.
NZNO recognises the linkage between workforce and the model of care. The ways in which Pacific communities interact with health-care services are influenced by familial and community structures and Pacific world views; this must be incorporated into development of model(s) of care.
Strategic actions
NZNO will:
- The NZNO Pacific Nursing Section has signalled its intention to develop a Pacific nursing strategic plan for its members, intended to advance the Pacific nursing contribution to health care and its future direction. The strategy will be underpinned by Pacific world views - including specific cultural beliefs, language, traditions, social structure and history, and its influence on nursing service delivery and health gains
- The NZNO Pacific Nursing Section will contribute to the development of a model of care that incorporates the influence of Pacific world views on community interaction with health-care services.
6.10 Mental health and addictions
Mental health is a critically important field of nursing, comprising many areas of expertise across the lifespan.
Mental health and addictions services in Aotearoa New Zealand are in crisis. Any crisis of this significance has multidimensional causes and occurs over a sustained period of time.
Services are overwhelmed throughout the country across primary, secondary and specialist services. A nationwide, total systems-approach is urgently required to re-calibrate investment, services and workforce. NZNO supports the Government’s Inquiry into Mental Health and Addictions (announced January 2018). The inquiry’s findings are due to be reported in October 2018.
NZNO position on mental health and addictions services
- The mental health and addictions services across the country is underfunded
- The parameters for service provision need re-setting, ie who gets what services, when
- The waiting times for services are unacceptable
- The fact that Aotearoa New Zealand has the highest rate of suicide in OECD countries is unacceptable, particularly the high rates for Māori, Pacific people, and adolescents/youth
- Mental health and well-being needs are increasing dramatically in Aotearoa New Zealand and internationally. Depression is a public health issue
- The number of people needing support for addictions is burgeoning, wait times are long, and treatment centres are few
- Serious staffing shortages across multidisciplinary teams are unacceptable and urgent attention is required
- The safety of mental health nurses is of significant concern, with verbal and physical abuse, long hours of work and moral distress because of the inability to provide optimal care, all compromising mental health nurses' well-being
- The ratio of qualified and experienced mental health nurses to mental health support workers is out of balance in many services. The lack of nurses has negative impacts for nurse, support worker and consumer
- Mental health service provision is fragmented and varies by region and in efficacy
- Talking therapies are a key feature of advanced mental health nursing practice. Increased funding for postgraduate advanced mental health nursing practice is needed
- There is a lack of services for youth with a history of criminal behaviour and who have an intellectual disability.
Current actions
- NZNO supports a review of mental health and addictions services, and will seek involvement at the highest level, including policy and service redesign
- NZNO supports service delivery co-design with consumers and culturally appropriate services
- NZNO will continue to promote healthy work environments and safe staffing for all NZNO members, and will be particularly aware of the challenging circumstances in the mental health sector.
Strategic actions
NZNO will:
- Actively pursue increased MoH, DHB and PHO investment in the mental health nursing workforce and services
- The NZNO Mental Health Nurses Section will work towards making mental health nursing an attractive choice for nurses at each stage of their career
- NZNO proposes to collaborate with other mental health nursing professional organisations to formulate a plan of action to raise the profile of mental health nursing to ensure patient safety, care and reasonable workloads are recognised as crucial to patient outcomes, and resourced appropriately.
6.11 Rural nursing
Most New Zealanders live and work in large urban areas, but Aotearoa New Zealand is, first and foremost, a rural country - by land mass, location of our primary industries and our history.
GP services have been declining in rural areas over several decades, largely due to the inability to attract GPs to work in rural areas. While this has had negative repercussions, it has been a catalyst for changing the prevailing model of care and extending the practice of other disciplines, particularly nursing. A lot can be learnt from this process.
NZNO is proud of the rural nurses who form a great part of our nursing heritage and continue to provide courageous and creative responses to health-care needs. Rural health nurses work in a special practice context. They practise in, and are part of, small, close-knit communities. Often these populations are socio-economically disadvantaged, transient (seasonal workers) and have high health needs. Aotearoa New Zealand’s increasing tourist numbers also equate to more demand on trauma and medical health care services in rural communities. There are often professional challenges working in rural communities – the greatest being patient confidentiality and the lack of anonymity for the nursing professional.
Rural nursing has been at the forefront of:
- Working collaboratively within health care teams – eg providing after-hours cover for team members
- Advancing practice in rural postgraduate education, clinical practice (eg P.R.I.M.E), and the use of technology such as telehealth, video links etc.
- Providing leadership, policy advice and influencing health decision makers
- Creating innovative nursing solutions in challenging situations (often with a minimum of funding).
The number of rural nurses is relatively small, however the significance of practice changes is remarkable. Some rural practices are now nurse-only and this is likely to continue in the future.
Current actions
- NZNO supports the principle of access to paid external professional supervision for all rural nurses working in autonomous roles
- NZNO supports the continuation and extension of the voluntary bonding programme to attract nurses to rural locations
- NZNO acknowledges the challenges of rural nursing, especially after-hours call-outs, locum cover for annual leave, and access to professional development
- NZNO supports rural nurse specialist and nurse practitioner roles in rural practice.
6.12 Gerontology nursing
Gerontology nursing is a specialty practice that addresses the unique physiological, psychological, developmental, economic, cultural and spiritual needs related to ageing and care of older adults.
Over 60 per cent of patients in acute settings are over the age of 65 and the fastest growing group of acute admissions are aged over 85.
The NZNO Gerontology Nurses Section is working to increase the visibility and value placed on gerontology nursing, through contributing to health policy, supporting gerontology research and by supporting educational, workforce and professional services to nurse members.
The In Safe Hands programme will focus on current staffing levels in aged care and the skill mix of staff in long-term aged care facilities. Staffing levels and skill mix have not been reviewed for many years and the voluntary nature of the existing guidelines often puts nurses and carers in situations where they cannot provide the quality care they want to provide and our older people deserve.
Current actions
- NZNO has initiated and is committed to the In Safe Hands programme. This is a partnership with multiple funding agencies to create a safe clinical and professional working environment for RNs and ENs with older persons
- NZNO supports a skilled, knowledgeable and professional workforce that is paid equitably. NZNO’s goal in the aged and primary health care sectors will continue to be pay parity with the DHB MECA pay equity rate when established.
Strategic actions
NZNO will:
- Recommend that the Health and Disability Commissioner includes the staffing levels and the context of the clinical environment, when considering breaches of the Health and Disability Code
- Recommend the gradual reduction of internationally qualified nurses in aged care and an increase in domestically qualified nurses
- Recommend increased funding for aged residential care, and home and community support budgets to increase RN hours/input to ensure safe care and support
- Recommend the nationwide implementation of support programmes for residential and community gerontology nurses as outlined in the MoH Showcasing Aged-care Nursing document.
6.13 Enrolled nurses
Over the last four decades, the EN education programme has suffered from a series of on-again, off-again changes to scope of practice, training content and duration, and even a name change. Nonetheless, enrolled nursing now has an improved and defined scope of practice, an established educational programme (New Zealand Diploma in Enrolled Nursing - level 5), is a regulated workforce and is poised to be a positive and enhanced workforce in health.
The lack of employment opportunities for ENs with the broadened scope of practice has been disappointing. The EN programme is well placed to create a critical mass of ENs as a valued and integral part of health service delivery for New Zealanders. Employers need to take the opportunity to employ ENs now, before health service demand increases further and there are fewer nurses available.
NZNO is committed to ENs as an integral part of the nursing team.
Current actions
- NZNO will continue to communicate the advantages of the expanded EN scope of practice and what it can bring to service delivery. Nurse leaders will have an important part to play in this process
- The Enrolled Nurse Section, will continue to implement the NZNO Enrolled Nurse Section Strategic Plan 2016-2021.
Strategic actions
NZNO will:
- Invest in and contribute to the increased understanding of the EN scope of practice, to nurse leaders and health employers
- Develop a marketing strategy to inform employment and health planning stakeholders on the scope of practice, capacity and capability and the range of services ENs can supply
- Encourage employers to use the support-into-practice framework and orientation programme to support new graduate ENs into the workforce. NZNO welcomes the agreement from Nurse Executives of New Zealand to endorse the framework
- Actively pursue dedicated funding for the support-into- practice framework for ENs. NZNO recommends the ACE process is used for this programme
- NZNO promotes the careful assessment of every nursing vacancy to establish what skill set is appropriate and required and, where possible, consider employment of ENs.
6.14 Nurse practitioners
Nurse practitioners' scope of practice has advanced education, clinical training and the legal authority to practise beyond the level of a registered nurse. They work autonomously and in collaborative teams across health-care settings to promote health, prevent disease, and improve population health outcomes.
Nurse practitioners may be the lead provider of health-care service for patients with complex health conditions. Their responsibilities can include diagnosis, assessment and treatment interventions, ordering and interpreting tests, prescribing medicines and patient admission and discharge.
The total number of nurse practitioners is still very low. NZNO has an aspirational target of 200-250 new nurse practitioners per year to improve access and health gain for patients, and to allow different models of care that support practice.
Current actions
- NZNO welcomes the amendments to the nurse practitioner scope of practice and the accompanying changes to the masters programme that prepares nurse practitioners for endorsement
- NZNO supports the enactment of the Health Practitioners (Replacement of Statutory References to Medical Practitioners) Bill and will ensure the resulting changes are operationalised.
6.15 Advanced practice
NZNO notes the progressive development of nurse prescribing in Aotearoa New Zealand. The successful diabetes nurses prescribing project and the establishment of the common conditions prescribing pilot is welcomed. However, there must be sufficient funding and support to create a critical mass of nurses who can make a difference to patient access, affordability and timeliness of treatment options to improve health outcomes in our communities.
Current actions
- NZNO supports the community prescribing pilot and looks to the advancement of RN prescribing. NZNO acknowledges the need for a pilot and for robust evaluation. However, it is also important to expedite progress towards a critical mass of nurses able to prescribe in the community.
6.16 Nurse endoscopists
NZNO welcomes the introduction of nurse endoscopists. To date, four nurses have commenced training in three DHBs since 2016. The postponement of the course in 2017 is a wasted opportunity to develop the endoscopy nursing workforce and to meet a clearly defined health need in Aotearoa New Zealand.
A critical mass of nurses is required to meet the rapidly increasing need for endoscopy services in general and the rollout of the national bowel screening programme in particular.
Strategic actions
The NZNO College of Gastroenterology nurses will:
- Continue to facilitate the introduction of nurse endoscopists wherever possible, identify potential challenges early and refer these to the NZNO professional services team.
6.17 Primary health care nursing
General practice in Aotearoa New Zealand is changing from small business units to medium- to-large business units, some with international ownership. This changing business structure requires shareholder return, as well as health care gain.
Primary care within general practice is working for those who can afford it and those who choose to access it. However, 500,000 New Zealanders have unmet health-care needs due to the cost of a GP visit.
Nursing services in the general practice team are influenced by several key factors:
- The employer model: the GP is the nurse’s employer and what the nurse does is mandated by what the employer allows
- The funding model: the nurse (and the GP) can be and often are constrained by the prevailing funding model
- The practice culture: each workplace has its own work environment culture, where the norms of “what happens around here” are strongly established.
Skilled, knowledgeable and experienced nurses, many with postgraduate qualifications, are practising within these structures. Yet a lot of these nurses would say they could practise more effectively if contractual, employment and funding mechanisms were different. Part of the problem is the large variability between practices. These issues have been articulated since the introduction of the Primary Health Care Strategy in 2001 but there has been little real will or effort to change the status quo.
There is a far more debate on the shortage of GPs than on the full utilisation of nurses in primary health care. This makes little sense in a climate of constrained resources (human and fiscal). The contribution of both professions must be respected and capitalised on to provide the best patient care.
To improve health gain in our community, primary health care nursing services (utilising nurses of all three scopes of practice) must be appropriately funded, reach across health and social care, be nationally/regionally/locally consistent and accessible to those who need it.
Investment in primary health care nursing will be required to increase the number and skill mix of nurses to undertake this work effectively.
For more information on primary care nursing workforce and model of care development see: NZNO College of Primary Health Care Nursing paper - Maximising the nursing contribution to positive health outcomes for the New Zealand population
6.18 Public health nursing service
The public health nursing service has a distinguished history in Aotearoa New Zealand, however successive restructurings since the 1980s has severely diminished the service.
The service is free, mobile, accessible, and works across school, home, and community. Public health nurses are seen as “community encyclopaedias” - practising across health determinants, across health and social sectors and at the level of both population and personal health. Their philosophy of care focuses on social justice, reducing inequalities in health and access to care, and commitment to te Tiriti o Waitangi.
Public health nurses work with many of Aotearoa New Zealand's most vulnerable children, tamariki and families, whānau and visit some of the coldest homes in the country. They work within an integrated health and social model.
Currently they are spread very thinly and do not have the critical mass necessary to meet the health needs they are educated and skilled to address. The competencies of this workforce are detailed in the Public Health Nursing Knowledge and Skills Framework.
Public health nurses fulfil all the strategic intentions of the New Zealand Health Strategy 2016. This potential needs to be realised.
Strategic actions
NZNO will:
- Advocate for a 50 per cent increase in the number of public health nurses by 2020. This workforce must be considered in model of care development. The critical mass of this workforce must be increased so it can make a difference to health outcomes for vulnerable families in Aotearoa New Zealand
- Work with the MoH to review contract specifications for public health nurses to enable these nurses to work to their full potential.
Healthy work environments and safe staffing
Healthy work environments
Poor work environments are a predictor of staffing losses. Issues that affect staffing retention include limited career opportunities, poor staff support, unsafe staffing, resourcing constraints, being left out of decision making, constant changes, and issues related to leave and shifts.
6.19 Safe Staffing Healthy Workplaces (SSHW) Unit
The SSHW Unit is part of the Central Technical Advisory Services. It was established in 2007 to develop a programme to implement the recommendations from the 2006 Report of the Committee of Inquiry on Safe Staffing Healthy Workplaces.
Achieving staffing that closely matches the needs of patient care, 24 hours a day, seven days a week, is essential to achieve optimum patient outcomes. It is also essential for the health and well-being of nurses and midwives. Ensuring there are sufficient nurses and midwives to provide safe, quality patient care is a fundamental goal for all who manage nursing and midwifery services, regardless of the setting.
The variable nature of the demand for health care and the relatively fixed nature of the nursing and midwifery workforces are characteristics common to all health services. These characteristics make it difficult to achieve a close match between workload and staffing.
This is a national and international challenge.
The diagram below represents the fundamentals underpinning safe staffing and healthy workplaces for nursing and midwifery staff.
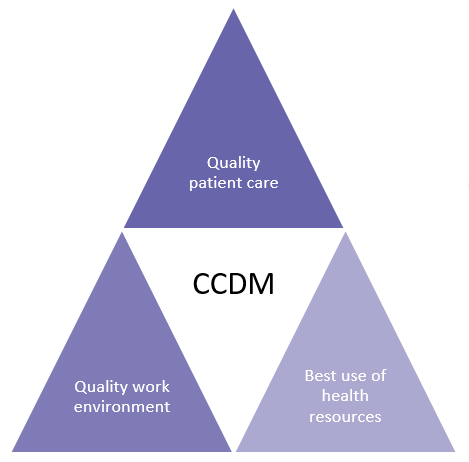
© MoH 2017 (used with permission)
NZNO’s safe staffing healthy workplace campaign is working to implement CCDM into DHBs. The CCDM programme matches patient demand with staff capacity, to ensure the right number of staff and the right mix of skills. A partnership between DHBs and NZNO and the other health unions is key to the successful implementation of the CCDM programme.
Key aspects of the CCDM programme
| Staffing methodology |
Variance response-management |
Core data set |
| The right people, the right place… the right care |
CCDM tools to help keep staff and patients safe and promote better use of resources. |
CCDM contributes to attainment of the Health and Disability Sector Standards |
| 1. The right people, the right place…the right care! |
1. In the moment and over time |
1. A balanced set of measures |
|
2. Provides data and evidence on which to base successful staffing models
|
2. Enable variance to be managed well, every time |
2. Measuring the impact of CCDM on your workload and workflow |
| 3. An independently validated process for establishing budgeted full-time equivalent staff |
3. Effective variance response management = early detection, rapid assessment and effective response |
3. Is about people, process and data from the floor to the board |
6.20 Safe staffing and care rationing
Care rationing - the ‘withholding or failure to carry out necessary nursing tasks due to inadequate resources such as time, staffing level, and/or skill mix’.
Nursing staff are concerned about staffing levels; they are stressed, distressed and anxious about their ability to deliver safe and effective care in an environment that is not properly resourced.
Care rationing is an ethical dilemma that nurses face every day. The conscious decision to prioritise some care and to drop off nursing tasks deemed to be lower risk is draining, demoralising and exposes nurses professionally and legally.
Care rationing is both a service quality and patient safety issue. Care rationing can result in falls, infections and pressure injuries, longer recovery times and even serious harm or death. It incurs significant costs and intensive resources.
The NZNO Position Statement on Care Rationing pulls together the evidence to show care rationing is happening. The statement puts forward solutions needed to make sure every patient gets the right nursing care, in the right place, at the right time, by the appropriate member of the nursing team.
Care rationing can be observed at the macro level where health funding is inadequate. At the micro level it can be seen when two patients require an intensive care unit bed but only one bed is available. The resulting prioritisation can lead to inequality in the health care service.
CCDM implementation has commenced in at least 14 DHBs, however, this has been slow and patchy. There is a serious risk of losing the confidence of nurses and midwives as a result, and this is contrary to the purpose of the programme.
Safe staffing and healthy workplaces are fundamentally important to nursing and midwifery, as they lead to workforce sustainability and safe patient outcomes. The failure to make progress on safe staffing and healthy workplaces is inexcusable. A renewed commitment to, and political will to enable safe staffing and healthy workplaces is needed to ensure the health workforce, and nursing and midwifery in particular, are supported by CCDM. This a high priority for NZNO.
Current actions
- NZNO endorses the draft ICN Position Statement on Safe Nurse Staffing Levels (2017).
Strategic actions
NZNO will:
- Support the implementation of CCDM in all DHBs by the agreed timeframe of June 2021
- Work in partnership with DHBs to ensure progress reporting on CCDM implementation (including the outcomes of FTE calculations) is managed in accordance with the requirements of the Safe Staffing Healthy Workplaces Governance Group and the Ministry of Health
- Use evidence from CCDM to inform DHB funding models.