A “Model of care” broadly defines the way health services are delivered. It outlines best practice care and services for a person, population group or patient cohort as they progress through the stages of a condition, injury or event.
The model of care is of critical importance. It is how services and health resources for the population of Aotearoa New Zealand are planned and allocated. However, nurses have been absent from decision-making and design phases of model-of-care development.
Nurses have not been involved or influenced the allocation of resources and must contend with the consequences of poor funding decisions, leading to sub-optimal care for patients.
3.1 Current context – the model of care in Aotearoa New Zealand
In a rapidly evolving health environment characterised by new knowledge and technology, growing health inequities and an increasingly diverse and ageing population, there is near unanimous recognition that current models may not meet future need and that new approaches are needed.
The challenge is to identify new, evidence- based models, and to coordinate the various approaches, ideas, and interventions (including changes to funding mechanisms) to ensure a cohesive platform for implementation.
The MoH New Zealand Health Strategy 2016 provides a rationale for action for the NZNO model of care:
- when demand changes, service mix and design may not change quickly enough
- some funding arrangements contribute to disparities between groups in their access to services and sometimes widen the gap in unmet need
- funding and contracting arrangements often encourage health services to keep doing things as they have always done them, or to inhibit evolving care requirements as they do not fit into restricted funding parameters.
The model of care always involves people and money.
Features of current funding and models of care in Aotearoa New Zealand:
- Lack of nursing input at the decision- making table
- A power and leverage base that consolidates the biomedical model, undermining public health/population models of health
- A strong conservative culture
- Medical hegemony and assumed superiority
- An internally regulated market to create a persistent state of medically “scarce resource” and the economic and industrial advantage this creates
- Promotion of innovation takes place in an essentially risk-averse environment.
3.2 We can improve model of care development
The bio-medical model of care has been politically acceptable and impenetrable to change - a situation that is historically embedded and self-reinforcing.
Human and fiscal resources in the Aotearoa New Zealand health system have been funnelled primarily through a series of institutions, eg MoH to DHB to hospitals, primary health organisations (PHOs), general practice, aged care and non-governmental community organisations. This is based on a business model that combines government funding and a co-payment patient charge at primary health care level, combined with a western biomedical approach to health care.
The model of care is the mechanism of power that is used to drive and produce both business and health gain. This, however, does not necessarily equate to equal gain between health provider and health consumer.
A health economics perspective is essential to allocate health resourcing in the best way to achieve improved health and social outcomes. It means the business model cannot lead the model of care (as occurs at present) but should accompany it, to meet changing contexts and population health needs, in the most cost-effective manner. It is also vitally important that an equity lens is applied to business models.
“Although the equity word is used freely within medical professional circles, the control of the primary health sector is shifting to a series of semi corporate, corporate, and international business entities… The (primary health care) sector was built on a small business model, and is fast becoming a large corporate model, with its focus on shareholder value rather than health equity.” ~ Don Matheson, 2016
3.3 What can nursing contribute to a model of care?
Nursing is a large, regulated, professional and skilled workforce. Nursing is dynamic, adaptable and can be rapidly deployed.
Nurses must be culturally competent. Cultural safety, te Tiriti o Waitangi and Māori health and nursing practice are required and audited components of each nursing curriculum. Additionally, NCNZ sets standards for continuing competence (including cultural competence) every nurse must demonstrate as part of their annual practising certificate.
Nurses work across the lifespan and the health/wellness continuum, and can express their practice in health, social and psychological health outcomes for New Zealanders.
Models of care – the nursing view
|
Nurses promote
|
- Aligning the model of care with community need
|
|
Nurses have
|
- From the turn of the 19th century, worked and are working in countless models of care
- The motivation to embrace new models of care, including technological change
- Been constrained by structural and funding barriers, a rigid ideology and the focus on a western biomedical model of care.
|
| Nurses welcome |
- The investment in the nurse practitioner role, and the effects of this workforce on safe patient health outcomes and service satisfaction
- The introduction of RN prescribing. Nurses look forward to the development of a critical mass of RNs prescribing for the health gain for all New Zealanders
- The evolution and ongoing development of whānau Ora services
- The development and implementation of Māori nursing frameworks, and Māori health models
- Models of care for rural health that are flexible and aligned to community need.
|
|
Nurses need
|
- The ability to work within a home-based model of care
- The ability to provide relational, humanistic and evidence-based care that results in positive behavioural change
- The opportunity to deliver services that improve health outcomes in a cost effective way (value and high performance)
- To continue interdisciplinary work and services as an integral part of their role
- Relocation of centres of care to populations with highest need
- Investment in ongoing cultural learning and training
|
| Nurses are inhibited by |
- Structural power (nurses are not at the decision-making table when services are designed)
- Funding and contracting mechanisms not suited to nursing philosophy or work mode
- A hierarchical model of care where medicine is the dominant paradigm.
|
3.4 Strengthening and supporting the whānau Ora model of care
whānau Ora is an inclusive approach to providing services and opportunities to whānau. It empowers whānau as a whole, rather than focusing on individual whānau members and their problems.
whānau Ora Outcomes
- whānau are self-managing and empowered leaders
- whānau are leading healthy lifestyles
- whānau are confidently participating fully in te Ao MāoriMāori (the Māori world)
- whānau and participating fully in society
- whānau are economically secure and successfully involved in wealth creation
- whānau are cohesive, resilient and nurturing
- whānau are responsible stewards of their living and natural environment
Adapted from https://www.tpk.govt.nz/en/whakamahia/whānau-ora/why-whānau-ora
whānau Ora recognises the best solutions to family challenges come from Māori families themselves. Māori families are supported to achieve their aspirations in education, training, economic development, health, participating in the community, developing cultural capital, strengthening identity and family development.
“The opportunity lies within the whānau Ora initiative for whānau to be navigated out of poverty, through support provided to whānau and the challenge laid down for institutions to become culturally responsive.” ~ Fiona Cram
Strategic actions
NZNO will work with external stakeholders to ensure:
- the evolution of the whānau Ora model of care is promoted, involving Māori nurses who work to the fullest extent of their scope of practice
- dissemination of best practice examples of Māori nursing models of practice
3.5 Developing a model of care for Aotearoa New Zealand nursing services
The NZNO vision statement ‘2020 and Beyond: a Vision for Nursing’ outlines the following aspirations for a model of care for Aotearoa New Zealand:
- Innovative and flexible models of care that are person-centred and are developed and evaluated by nurses.
- Technology, enhanced communication, and new treatment modalities will be utilised to ensure models of care are appropriate, cost effective and meet the needs of all people.
- People will be consulted about the models that best meets their needs, and nurses will work collaboratively with other health professionals to meet these needs.
- The principles of whakawhānaungatanga, manaakitanga, rangatiratanga, oritetanga and wairuatanga will continue to guide professional nursing practice.
Some major shifts are required in the way our health-care system operates to achieve these aspirations. This situation is outlined below.
Major shifts required to improve the model of care
|
Historical
|
Contemporary |
|
Biomedical model
|
Biophysical and psychosocial health orientation
|
Medical home
|
Health is in the person’s home, health is everywhere - there is no wrong door |
|
Funding and contracting
|
Flexible funding and improved contracting |
| Cost |
Investment |
| Economic rationalism |
Healthy population growth = economic growth |
| Innovation at the margin |
Innovation in mainstream |
| Nurses as a unit of production |
Nurses as the solution to sustainable, high-quality services |
| Western-centric model |
Holistic models of care incorporating Te Ao Māori worldview |
The foundations for the model of care for nursing will include:
- Aligning nursing services with community need and working across the determinants of health
- Incorporating universal health coverage
- Cost-effective service provision
- Holistic models of care incorporating Māori world views and covering biophysical and psychosocial health
- Incorporating existing and expected developments in information technology
- A generalist and population focus
- Fully utilising the capability and capacity of the nursing workforce
- Recognising existing innovative and effective models of care operating in Aotearoa New Zealand
- A focus on Māori populations, incorporating Māori models of care and worldview
- A focus on Pacific populations, incorporating Pacific models of care and worldviews
- A focus on staff cultural competence to ensure excellence of clinical and professional practice
- Tiriti-based practice, including concepts of agency, authority and the ability of Māori to make decisions for themselves. This requires the development of an effective voice, as well as determination and confidence, supported by evidence, resources and technical skills.
- A lifespan approach, a family orientation, but an all-population overview
- Having a critical mass of nurses working where people live, work, play, age and die.
Preventative care
Preventative care and health promotion are integral parts of a model of care. This is illustrated in the ICN diagram below. The second tier from the bottom of the pyramid involves health literacy, health promotion, self-management and strategies for positive health decision making. The third tier refers to lifelong health (eg healthy eating, active lifestyles, and living environments).
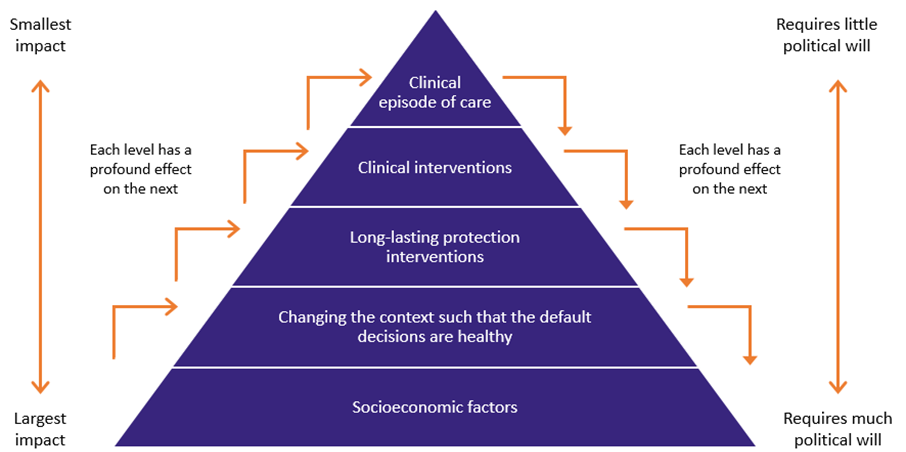
Source: ICN, 2017.
This diagram illustrates how the largest gains in health improvement can be made through activities at the broader, population-based levels. This is also where the greatest level of political will is required - a key consideration in the NZNO Strategy for Nursing.
Strategic actions
NZNO will:
- Create a terms of reference for an advisory group with expertise within Te Runanga, college and section networks, to prepare a nationwide core model of care for Aotearoa New Zealand nursing services. This will include options for shared services, funding and contractual mechanisms and be completed within a year of release of the NZNO Strategy for Nursing
- Form the internal expert advisory group for model of care development. Additional expertise will be co-opted as necessary
- Undertake a stocktake of nurse-led services (of all types) and innovations (current and past) and disseminate them through the NZNO website.
3.6 Innovation
Innovation is integral to providing improved and more appropriate health, social and psychological care to communities and an essential aspect of the nursing model of care for Aotearoa New Zealand.
The main driver for nurses to utilise innovative practices is to improve patient experience, health outcomes and nursing practices. Whatever the service design, it must be acceptable to the user, feasible to implement at scale and sustainable.
More money and a different funding approach is needed to support innovative practice. Many past innovative nursing practices and model of care enhancements were not sustained due to inadequate funding.
Funding of nursing innovation: historical and contemporary approaches
|
Historical funding approaches
|
Contemporary funding approaches |
| Underfunded at commencement |
Appropriately funded at commencement |
| Annual contract |
Multi-year contract |
| Evaluation takes place too early in service innovation development (if at all) |
Intermediate evaluation or action research methodology |
| Evaluation funding not incorporated into total funding at service innovation commencement |
Adequate evaluation funding at service innovation commencement |
| Service innovation is easy to discontinue when funding is short |
Services are usually maintained via high community engagement |
| Service innovation at the margins does not become mainstream |
Service innovation disseminated and is able to be replicated at scale. |
NZNO supports a human-centred approach and design thinking methodology for innovation
Design thinking takes a human-centred approach to creating and implementing innovative programmes - integrating patient needs, alternative approaches and technologies, and wise and cost-effective use of health funding.
Strategic actions
NZNO will:
- Continue to seek and share innovative practices with members through its website, communications and publications, and through Te Runanga and the NZNO colleges and sections
- Provide expertise on proposal documentation, including review of financial modelling for innovative practice, bicultural service design or model of care proposals
- Use available and emerging information technology and data to drive innovation and decision making.
- Support investment in and the implementation of Māori nursing innovation.